All Publications
Health Care Expenditures in California
Document
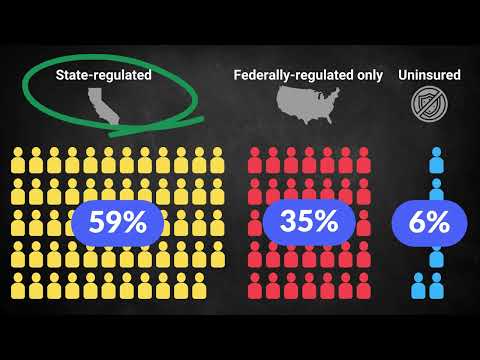
Sources of Health Insurance in California in 2025
Pharmacy Benefit Managers: The Basics
Enrollee Health Care Expenditures: Premiums, Cost Sharing, and Noncovered Expenses
Preventive Services in California
Document
Basic Health Care Services
Document
Essential Health Benefits
Document